The US vaccinated more than 4 million people on a single day on April 3, 2021. With countries ramping up vaccination against COVID-19 all over the world, there remain numerous questions regarding the COVID-19 vaccine. This article attempts to answer questions related to the Pfizer-BioNTech and Moderna vaccines which were the first and second vaccines respectively, to be approved by the Food and Drug Administration (FDA) for use against COVID-19.
The source of a lot of the answers to these questions is from the recommendations of the Advisory Committee on Immunization Practices (ACIP) for COVID-19 vaccines published by the Centers for Disease Control and Prevention (CDC).
The Pfizer-BioNTech and Moderna vaccines are nucleoside-modified mRNA vaccines encoding the prefusion spike glycoprotein of SARS-CoV-2. SARS-CoV-2 is the virus that causes coronavirus disease 2019 (COVID-19). The Pfizer-BioNTech COVID-19 vaccine consists of two doses (30 μ_g, 0.3 mL each) administered intramuscularly, three weeks apart. Vaccination with the Moderna COVID-19 vaccine consists of two doses (100 μ_g, 0.5 mL each) administered intramuscularly, 1 month (4 weeks) apart. The vaccines can be taken by anyone over 16 years ( Pfizer-BioNTech) or 18 years (Moderna) of age for the prevention of COVID-19 as per ACIP interim recommendations.
Let’s take a look at the common questions and clarify your doubts.
How many doses of the Pfizer-BioNTech or Moderna COVID-19 vaccine do you need to take?
You need to take two doses of the Pfizer-BioNTech (30 _μ_g, 0.3 mL each) administered intramuscularly, three weeks apart. This is a two-injection vaccination. After the first shot is given, you have to get the second shot within 17 to 21 days. If you happen to go past 21 days, you need to get the second injection as soon as possible, preferably within 25 days. In that situation, you do not need to repeat the first dose, you just take the second shot.
Similarly for the Moderna vaccine, you need to take two doses (100 _μ_g, 0.5 mL each) administered intramuscularly, 1 month (4 weeks) apart. If you happen to go past 28 days, you need to get the second injection as soon as possible, preferably within 32 days of the first shot.
You need to complete the second shot with the same product. So, if you took the Pfizer-BioNTech vaccine in the first dose, you need to take the Pfizer-BioNTech for the second dose as well. The same applies to the Moderna vaccine. It is important to note that two doses need to be taken to provide adequate protection against COVID-19. A single dose is not sufficient.
What side effects to expect after vaccination?
Pain at the injection site or you might have fevers or chills, fatigue, or muscle aches within the next 24 hours. That’s to be expected because it’s stimulating your immune system to have an immune response against the vaccine. If you experience these side effects on the first shot, expect to get them on the second shot as well. It may even be more intense with the second shot.
You should also know that it is okay to take medications for reducing fever or for pain in these post-vaccination symptoms. You should not take Tylenol (acetaminophen) or NSAIDs as routine prophylaxis due to a lack of information on the impact of medication use on vaccine-induced antibody responses. So only use if needed.
How effective are the Pfizer-BioNTech and Moderna vaccines in preventing COVID-19?
Currently, at this point, all we know is that both vaccines are very effective at preventing COVID-19 disease. The Pfizer-BioNTech vaccine is about 95 percent effective and the Moderna vaccine is about 94 percent effective at preventing COVID-19. There’s no vaccine that’s 100 percent effective.
Do you need any COVID-19 tests prior to vaccination?
You do not need to get a COVID-19 test. Either a PCR or an antigen test nor do you need to get antibody tests to see whether or not you can get the vaccine.
What if you had a previous COVID-19 infection?
Regardless of whether or not you’ve had a previous infection, you should get vaccinated. Whether or not you had severe COVID or even had asymptomatic COVID, but you found out later that you were positive, you should still get the vaccine.
What if you received antibody or plasma therapy during a previous COVID-19 infection?
We don’t have any data on these vaccines in people who have received antibodies, monoclonal antibodies, or plasma treatment for COVID-19 in the past. So it’s potentially advisable to wait 90 days after you received any kind of plasma or antibody therapy. This is to make sure that those antibodies are out of the system before getting the vaccination.
What if you have a current COVID-19 infection?
If you have a current infection with COVID-19, you should not get the vaccine. You should wait at least 14 days after the infection and you’re done with isolation, before considering getting the vaccine. Current evidence suggests that reinfection, while it can happen, is not common within 90 days after the initial infection. So if you wanted to delay vaccination until the end of the 90 day period after your first infection, you could do that if you wanted.
What if you have underlying medical conditions?
As long as you don’t have any contraindications to the vaccine, like allergies, etc., you can take the vaccine. There seems to be similar safety and efficacy in phase two and three trials in the Pfizer-BioNTech and Moderna vaccines for people with underlying medical conditions. These include immunocompromised patients like patients with HIV or other immunocompromised medical conditions like cancer.
Since both these are not live vaccines, they can be safely administered to people with underlying medical conditions. We need to remember that patients with HIV or immunocompromised conditions should be counseled. There’s no real available data to establish the safety or efficacy of the vaccine in these groups, but currently, they’re not being excluded at this point.
Can you take the COVID-19 vaccine if you are pregnant?
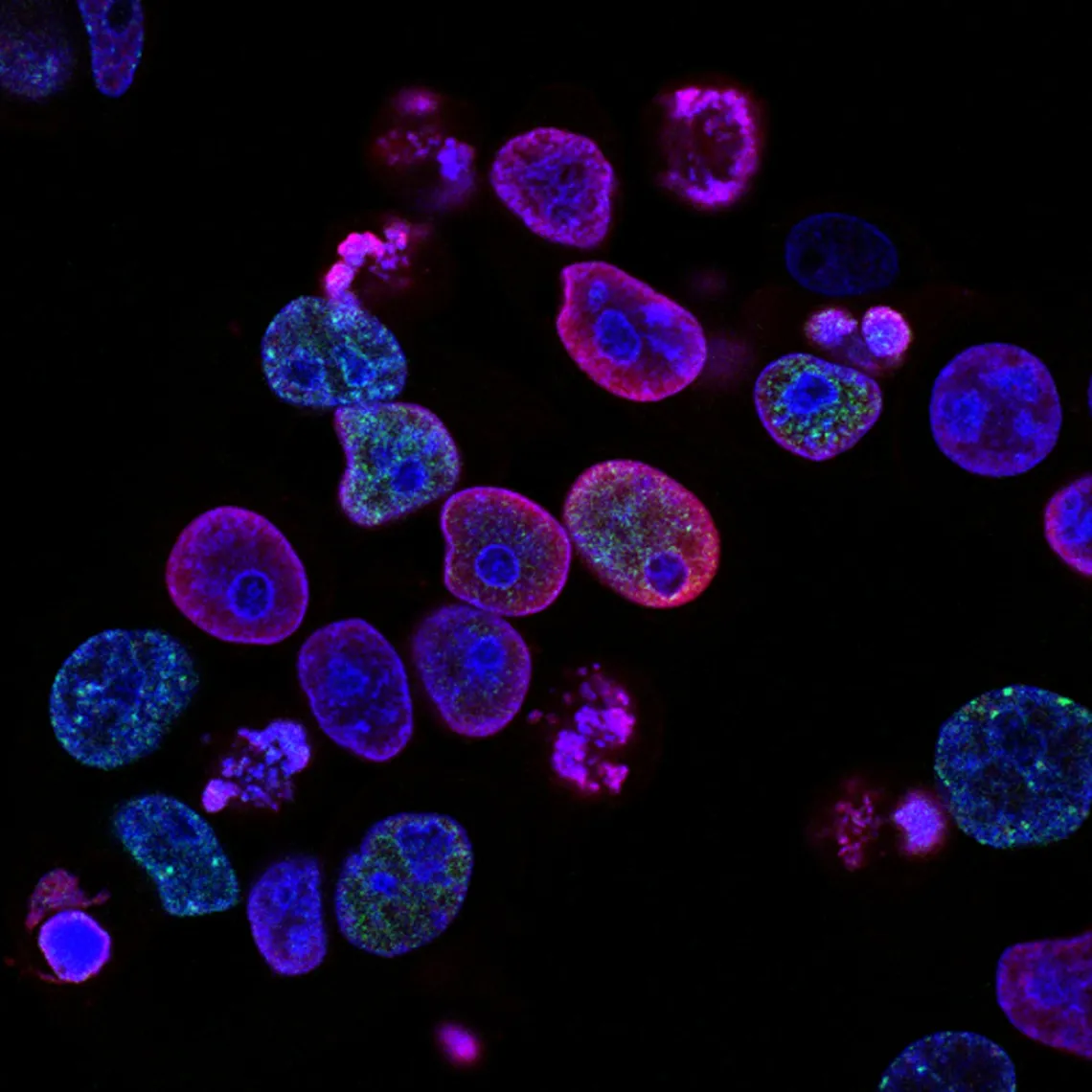
We currently have no data on safety or efficacy in pregnancy, but studies are ongoing. However, there were some people in the vaccine arm of the clinical trial that did get pregnant, so that data should be available soon. Generally, we don’t like to give live vaccines in pregnancy. The Pfizer-BioNTech and Moderna vaccines are not live virus but Messenger RNA (mRNA) vaccines. mRNA vaccines are broken down quickly in the cells. They do not enter the nucleus of the cell. They do not change your DNA.
On the flip side, emerging data is showing that patients who are pregnant seem to have a worse course of COVID. There has been an increased risk of adverse pregnancy outcomes like preterm birth in COVID patients.
The current recommendations are that there should be a discussion with the pregnant woman before vaccination. So that she can make an informed decision of the risk of contracting COVID-19 during pregnancy versus efficacy and side effects of the vaccine.
If a pregnant woman decides to take the COVID-19 vaccine and she develops a post-injection fever, the recommendation is to take acetaminophen due to fever being associated with adverse pregnancy outcomes. Currently, the recommendation is against routine testing for pregnancy in child-bearing age women before giving a COVID-19 vaccine.
Should you take the COVID-19 vaccine if you are breastfeeding?
There is no safety data with COVID-19 vaccine or effect of mRNA vaccines on breastfed infants or on milk production. Again an mRNA vaccine is not thought to be a risk factor for the breastfeeding infant. The current recommendation is if a lactating woman is part of a group, like a healthcare worker that has been recommended to receive the COVID-19 vaccine, she may be vaccinated if she chooses.
What are the long-term side effects of the COVID-19 vaccine?
Most of the adverse effects due to the vaccine occur within 6 weeks of taking the vaccine. This is why the FDA asks the vaccine manufacturers to provide 8 weeks of safety data after the last dose.
In the case of mRNA vaccines ( Pfizer-BioNTech and Moderna vaccines), the mRNA in the vaccine is broken down pretty quickly by the cells. But, even if for some reason the vaccine mRNA is not completely broken down, the mRNA stops making the protein within about a week, regardless of the body’s immune response to the protein.
What are the recommendations in terms of giving the COVID-19 vaccine with the flu shot?
The COVID-19 vaccine should be administered with a minimum interval of 14 days either before or after administration of any other vaccine, and that includes the flu shot.
How do you make sure that you don’t get tested positive for SARS-CoV-2 because you got vaccinated?
The good news is the Pfizer-BioNTech or Moderna COVID-19 vaccine will not affect the results of a SARS-CoV-2 nucleic acid amplification test, otherwise known as a PCR test or antigen test. However, if you want to check for antibodies, this vaccine induces both a humoral (antibody) response and a T cell response. The Pfizer-BioNTech or Moderna vaccine mRNA codes for the viral spike protein. So, if the antibody that you’re testing for is against the spike protein and it’s positive after the vaccination, you won’t be able to tell whether or not that positive antibody was a result of vaccination or previous infection with COVID-19.
Now, because the mRNA vaccine codes for the spike protein but if you make an antibody against the nucleocapsid protein, which is another portion of the virus, and if you are positive for that, then you can say it’s not from the vaccine, but you actually had an infection with COVID-19 virus SARS-CoV-2.
So, after you get vaccinated, it’s important to let people know that you have taken the vaccine. If they want to check to see whether or not you’ve actually been infected with the virus itself, they should be checking for the nucleocapsid protein antibody.
Should you continue to take precautionary measures like washing your hands, wearing masks, and social distancing after taking the second dose of the COVID-19 vaccine?
Yes, you still need to do ALL of the above until we reach herd immunity, or until we have well-established data that shows that COVID-19 vaccines can actually stop viral transmission.
Can the Pfizer-BioNTech or Moderna vaccine prevent transmission of the SARS-CoV-2 virus?
“A vaccine that is highly effective at preventing people from acquiring the infection in the first place would help to reduce transmission”, says Larry Corey, an internationally renowned expert in virology, immunology, and vaccine development at the Fred Hutchinson Cancer Research Center in Seattle, Washington.
To really prove whether vaccines prevent transmission, contact tracing is important. Researchers are tracking the close contacts of vaccinated people to see whether they are being indirectly protected from infection.
Vaccines are helpful in preventing COVID-19 and should be taken to protect yourself and others unless contraindicated. You should continue to take precautions even if you have received two doses of the vaccine. Hopefully, I have answered most of the commonly asked questions regarding the Pfizer-BioNTech and Moderna vaccines.
If you have not yet taken the vaccine, get yourself vaccinated against COVID-19. Stay safe during the pandemic.
Please share if you found this post helpful. Help to spread knowledge and dispel misconceptions about COVID-19.